How Machine Learning Models Detect Coding Errors and Predict Billing Issues
Introduction
Medical coding errors cost healthcare organizations billions annually through claim denials, compliance penalties, and revenue leakage. Manual review misses subtle inconsistencies, outdated codes, and complex billing logic errors, while traditional rule-based systems struggle with nuanced judgment.
Machine learning enhances medical coding by analyzing patterns across millions of claims, detecting anomalies, and supporting billing issues prediction before submission. It adapts to coding changes and provides intelligent recommendations, continuously improving accuracy and reducing errors.
In this blog, we discuss how machine learning models detect coding errors and predict billing issues, helping healthcare organizations optimize revenue cycle management and reduce costly mistakes effectively.
How ML Detects Medical Coding Errors
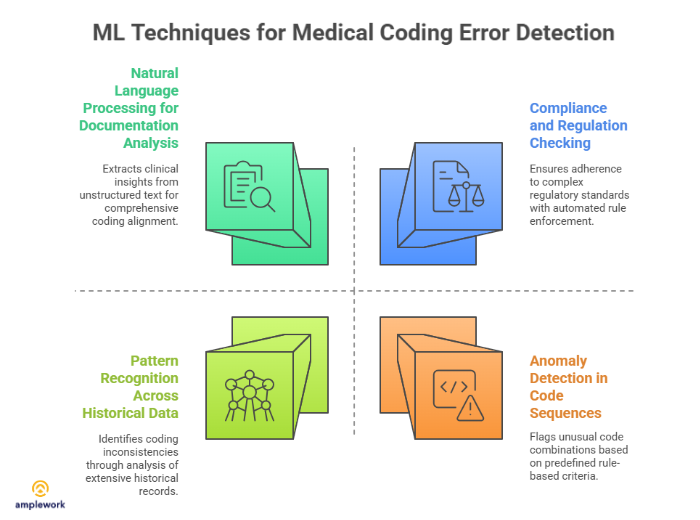
Pattern Recognition Across Historical Data
AI in healthcare enhances coding error detection by analyzing thousands of historical claims, identifying patterns in correct coding versus errors. Machine learning models learn relationships between diagnoses, procedures, modifiers, and appropriate codes, catching inconsistencies that manual review often misses.
Pattern analysis includes:
- Diagnosis-procedure correlation validation
- Modifier usage appropriateness checking
- Code combination logic verification
- Provider-specific pattern learning
- Specialty-based coding norms
Models trained on your organization’s data understand your specific coding patterns and identify deviations indicating potential errors.
Anomaly Detection in Code Sequences
Coding error prediction uses anomaly detection, identifying unusual code combinations or sequences that likely indicate mistakes. It uses machine learning in medical coding to flag anomalies. If a code rarely appears with certain diagnoses or procedures, machine learning flags it for review before claim submission.
Anomaly detection covers:
- Unusual code pairings identification
- Frequency-based outlier detection
- Contextual appropriateness assessment
- Statistical deviation flagging
- Sequential logic validation
This catches errors that technically follow rules but represent unlikely or inappropriate coding choices in context.
Natural Language Processing for Documentation Analysis
Advanced systems use NLP to analyze clinical documentation and compare it against assigned codes. Machine learning for medical billing extracts clinical facts from notes, matches them to coded diagnoses and procedures, and identifies discrepancies suggesting coding errors or missed opportunities.
Documentation analysis includes:
- Clinical entity extraction
- Diagnosis mentions identification
- Procedure description matching
- Code-documentation alignment verification
- Undercoding opportunity detection
This ensures codes accurately reflect documented clinical reality rather than just passing technical validation rules.
Compliance and Regulation Checking
Machine learning in medical coding helps models stay current with coding guidelines, payer-specific rules, and regulatory requirements. They automatically flag codes or combinations violating current regulations, outdated codes, or payer-specific restrictions that cause claim denials.
Compliance checking covers:
- Code validity verification
- Coverage rule application
- Medical necessity validation
- Bundling rule enforcement
- Payer-specific requirement checking
Automated compliance checking catches regulatory issues before expensive claim denials and potential audits.
How ML Predicts Billing Issues
Claim Denial Prediction
Machine learning models analyze claim characteristics, predicting denial likelihood before submission. These predictions identify high-risk claims needing additional review or correction, preventing costly denial-resubmission cycles.
Denial prediction examines:
- Historical denial pattern analysis
- Payer-specific rejection trends
- Code combination risk assessment
- Documentation completeness evaluation
- Prior authorization requirement detection
Proactive denial prediction allows correction before submission rather than expensive appeals after rejection.
Revenue Leakage Identification
Error detection in coding extends to identifying undercoding and missed charges. ML models recognize when documentation supports higher-value codes or additional billable services that went uncoded, preventing revenue loss.
Revenue optimization includes:
- Documentation-supported code upgrades
- Missed service identification
- Appropriate modifier suggestions
- Bundling opportunity detection
- Query generation for clarification
This protects revenue while maintaining coding accuracy and compliance.
Reimbursement Forecasting
Billing issues prediction includes estimating expected reimbursement amounts and flagging claims with unusual payment patterns. Discrepancies between expected and likely reimbursement indicate potential coding errors or billing problems.
Reimbursement analysis covers:
- Expected payment calculation
- Reimbursement variance detection
- Underpayment identification
- Payment pattern anomalies
- Contract compliance verification
Early identification of reimbursement issues enables quick resolution before patterns become established.
Prior Authorization Requirements
ML models predict which services require prior authorization based on procedure codes, diagnoses, payer rules, and historical patterns. This prevents claim denials from missing authorization and delays in patient care.
Authorization prediction includes:
- Payer-specific rule application
- Procedure authorization likelihood
- Documentation requirement identification
- Timeline estimation
- Alternative code suggestions
Proactive authorization management reduces denials and administrative burden significantly.
Also Read : AI Translation Proof of Concept: Step-by-Step Setup Guide
Implementation Benefits
- Reduced Claim Denials: Catching errors before submission dramatically reduces denial rates and associated rework costs.
- Improved Revenue Cycle: Faster, cleaner claims accelerate cash flow and reduce days in accounts receivable.
- Enhanced Compliance: Automated regulation checking reduces audit risk and compliance violations.
- Increased Coder Productivity: ML handles routine validation, allowing coders to focus on complex cases requiring judgment.
- Continuous Learning: Models improve over time learning from corrections, denials, and new patterns.
- Cost Savings: Reduced denials, improved revenue capture, and increased efficiency deliver measurable ROI.
Why Choose Amplework?
At Amplework Software, we develop custom machine learning solutions for healthcare organizations to tackle coding errors and billing issues. Our team identifies high-impact opportunities where ML delivers measurable ROI in revenue cycle operations.
Our solutions cover coding error detection, billing issues prediction, claim forecasting, revenue optimization, and compliance monitoring. ML integrates seamlessly into workflows through AI automation services, delivering actionable insights to the right people at the right time.
Also Read : When to Hire Reinforcement Learning Developers for AI Projects
Final Words
Machine learning in medical coding transforms medical coding and billing from reactive error correction to proactive issue prevention. ML models detect coding errors, predict billing issues, and optimize revenue capture with accuracy beyond manual processes. Healthcare organizations implementing ML achieve faster reimbursements, fewer denials, improved compliance, and increased revenue, delivering measurable ROI and reliable results.


 sales@amplework.com
sales@amplework.com
 (+91) 9636-962-228
(+91) 9636-962-228