AI vs Manual Medical Coding: Accuracy, Productivity & Error Reduction Explained
Introduction
A medical coder reviews a patient chart, identifying diagnoses and treatments to assign the correct codes, a process taking 15–20 minutes per chart. Multiplied across thousands of daily encounters, this creates significant time, cost, and operational burden. Medical coding errors cost the U.S. healthcare system an estimated $36 billion annually (AHIMA, 2024). With an aging population and growing regulatory complexity, accuracy and speed are more critical than ever. In this blog, we discuss AI vs manual medical coding, cover the basics of medical coding, explore the hybrid model, and highlight key implementation considerations.
What Is Medical Coding and Why Does It Matter?
Medical coding translates patient encounters into standardized codes (ICD-10, CPT, HCPCS) used for billing, insurance claims, and healthcare analytics. Accurate coding determines reimbursement amounts, compliance with regulations, and data quality for clinical research.
The challenge: Human coders process complex medical documentation, apply constantly updated coding guidelines, and ensure compliance, all while maintaining productivity standards. It’s mentally demanding work where errors have significant financial and legal consequences.
Manual Medical Coding: The Traditional Approach
1. How Manual Coding Works
Certified medical coders review clinical documentation, physician notes, lab results, and procedure reports, then assign appropriate diagnostic and procedural codes. They must:
- Interpret complex medical terminology and abbreviations
- Apply coding guidelines and payer-specific rules
- Query physicians for clarification when documentation is ambiguous
- Stay current with quarterly code updates and regulatory changes
- Ensure code combinations follow compliance rules
2. Strengths of Manual Coding
- Contextual Understanding: Human coders understand nuance, clinical context, and physician intent that documentation may not explicitly state.
- Complex Case Handling: Unusual presentations, rare conditions, or complicated procedures benefit from human judgment.
- Query Generation: Experienced coders identify documentation gaps and request physician clarification to improve accuracy.
3. Limitations of Manual Coding
- Productivity Constraints: Even skilled coders process 20-30 charts daily, creating bottlenecks as patient volumes increase.
- Error Rates: Studies show manual coding error rates between 15-20% (AHIMA, 2023), including incorrect codes, missed diagnoses, and unbundling violations.
- Cost Structure: The average cost per manually coded chart is $3.50-$5.00 (Healthcare Financial Management Association, 2024), with higher complexity cases costing significantly more.
- Inconsistency: Different coders may code identical cases differently due to variations in interpretation and experience levels.
- Burnout Risk: Repetitive, high-pressure work contributes to turnover rates exceeding 30% in coding departments.
AI-Powered Medical Coding: The Modern Alternative
1. How Automated Medical Coding Works
AI medical coding systems use natural language processing and machine learning to analyze clinical documentation and automatically recommend appropriate medical codes. Advanced solutions leveraging AI in healthcare typically employ:
- Natural Language Understanding: Extracting medical concepts, diagnoses, procedures, and relationships from unstructured clinical notes.
- Code Assignment Logic: Applying coding rules, guidelines, and payer requirements to suggest appropriate codes.
- Confidence Scoring: Indicating certainty levels for each suggested code, flagging uncertain assignments for human review.
- Continuous Learning: Improving accuracy over time by learning from coder corrections and new examples.
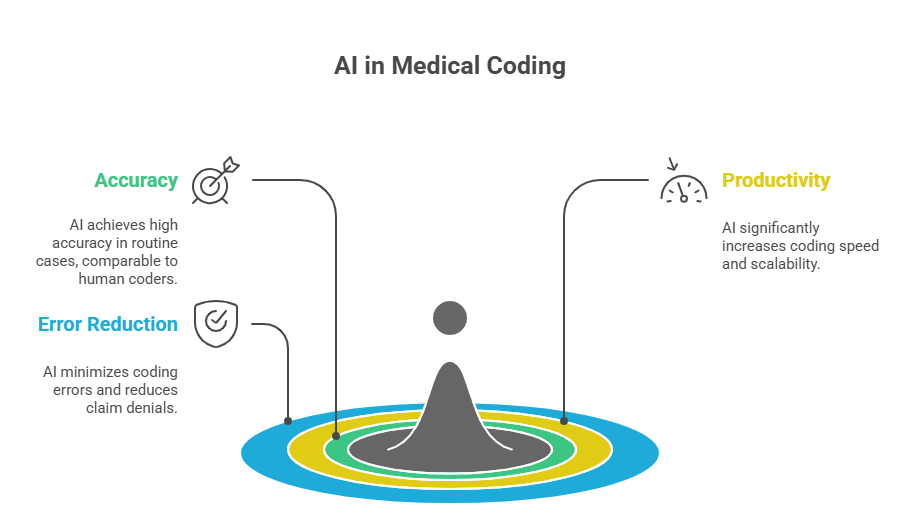
2. Automated Medical Coding Accuracy
AI coding accuracy has reached 85-95% for routine cases (Journal of AHIMA, 2024), comparable to or exceeding human coder accuracy for standard encounters. However, accuracy varies by:
- Case Complexity: Simple outpatient visits achieve 90-95% accuracy; complex inpatient cases with multiple complications see 75-85% accuracy.
- Specialty Areas: Well-documented specialties (cardiology, orthopedics) show higher accuracy than poorly standardized documentation areas.
- Training Data Quality: Systems trained on your organization’s specific documentation patterns perform better than generic models.
3. AI Coding Productivity Gains
The productivity difference between AI and human coders is substantial:
- Processing Speed: AI systems code charts in 30-90 seconds versus 15-20 minutes manually, representing 10-40x speed improvement.
- Scalability: AI handles volume spikes without additional staffing. During flu season or pandemic surges, systems scale instantly.
- 24/7 Availability: Automated coding operates continuously, eliminating backlogs from nights, weekends, or staff absences.
- Consistent Output: AI maintains consistent coding logic across all cases, eliminating variability between individual coders.
4. Error Reduction in Medical Coding
Medical billing errors decrease significantly with properly implemented AI:
- Coding Guideline Compliance: AI consistently applies current coding rules without lapses in knowledge or memory.
- Bundling/Unbundling Accuracy: Automated systems catch improper code combinations that humans miss under time pressure.
- Documentation Quality Feedback: AI identifies incomplete documentation, prompting physician queries before claims submission.
- Denial Prevention: Catching errors before claim submission reduces denial rates by 30-45% (MGMA, 2024).
A multi-specialty group reduced coding-related denials from 12% to 4.8% within six months of implementing AI coding with human oversight.
AI vs Manual Medical Coding: Comprehensive Comparison
| Factor | Manual Coding | AI-Powered Coding |
| Processing Speed | 15-20 min per chart | 30-90 seconds per chart |
| Daily Volume (per FTE) | 20-30 charts | 200-400 charts (with human review) |
| Accuracy (routine cases) | 80-85% | 85-95% |
| Accuracy (complex cases) | 85-90% | 75-85% |
| Consistency | Variable by coder | Highly consistent |
| Scalability | Limited by staffing | Instantly scalable |
| Adaptation to Changes | Training required | Model updates needed |
The Hybrid Model: Combining AI and Human Expertise
The most effective approach combines automated medical coding with human oversight:
- AI Handles Routine Cases: Straightforward encounters with high confidence scores proceed through automated coding without human review.
- Humans Focus on Complexity: Coders review complex cases, low-confidence assignments, and high-value claims requiring judgment.
- Continuous Improvement Loop: Human corrections train AI systems through AI model training, improving accuracy over time.
- Quality Assurance: Experienced coders perform random audits of AI-coded charts, maintaining accuracy standards.
This hybrid approach achieves the productivity gains of automation while preserving accuracy through human expertise where it matters most.
Implementation Considerations for Medical Coding Automation
- Integration with EHR Systems: AI must access clinical documentation seamlessly from electronic health records without workflow disruption.
- Specialty-Specific Training: Generic AI models require customization for specialty-specific terminology, procedures, and documentation patterns.
- Regulatory Compliance: Systems must maintain HIPAA compliance, audit trails, and meet payer-specific coding requirements.
- Change Management: Staff need training on working alongside AI, reviewing suggestions, correcting errors, and understanding confidence scores.
- ROI Timeline: Most organizations achieve positive ROI within 6-12 months through increased productivity, reduced denials, and faster reimbursement cycles.
Also Read : AI Development Roadmap: Steps to Build & Scale AI Systems
Conclusion
AI vs manual medical coding isn’t about replacement; it’s about augmentation. Combining automated medical coding with human oversight boosts productivity, reduces errors, and improves financial outcomes. Hybrid models help healthcare organizations stay ahead as coding volume and complexity grow.
Amplework’s AI automation services streamline coding workflows, enhance accuracy, and ensure compliance. By integrating seamlessly with existing systems, their solutions free coding teams to focus on higher-value tasks while delivering measurable operational and financial benefits.


 sales@amplework.com
sales@amplework.com
 (+91) 9636-962-228
(+91) 9636-962-228